Find Your Path: Therapy Options for Anxiety with Affirming, Culturally Aware Care
Anxiety can feel overpowering, but the right therapeutic approach from a therapist who affirms your identity can shift how you respond to worry, panic, and avoidance.
This guide walks through core approaches: Cognitive Behavioral Therapy (CBT), Acceptance and Commitment Therapy (ACT), Exposure Therapy, Dialectical Behavior Therapy (DBT), psychodynamic and interpersonal therapies, so that you and your mental health professional can see where each tends to help. You’ll get clear definitions, how each method creates change, practical exercises to try or raise with a mental health professional, and step‑by‑step tips for finding culturally sensitive care. We highlight how affirming therapy supports LGBTQ+ and BIPOC adults, and how telehealth and insurance navigation in New York and New Jersey can make care more accessible. After describing techniques and exercises, the article gives actionable next steps for locating an affirming therapist, including practical notes on insurance and affordability. Our goal is to leave you informed and ready to begin anxiety‑focused work with confidence.
What Is Cognitive Behavioral Therapy and How Does It Help Anxiety?
Cognitive Behavioral Therapy (CBT) is a structured, evidence‑based therapy that targets the connections between thoughts, feelings, and actions to reduce anxiety. CBT helps people spot unhelpful thinking patterns, test those beliefs with behavioral experiments, and decrease avoidance through graded exposure—changes that consistently lower symptoms across generalized anxiety disorder, social anxiety, and panic disorder. Typical CBT treatment involves weekly therapy sessions, collaboratively set goals, practice between sessions, and progress tracking; many people notice improvement within weeks to a few months. Knowing these core components makes it easier to recognize when a mental health professional’s approach aligns with CBT and how specific techniques might apply to your daily life.
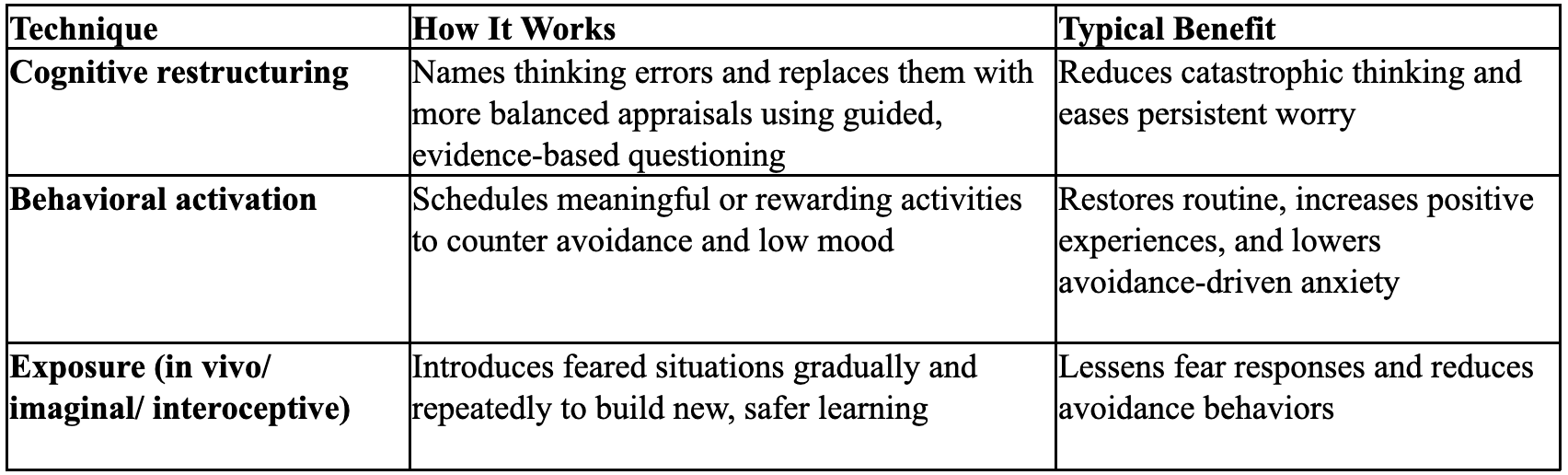
CBT uses several core tools mental health professionals combine to match a person’s anxiety profile. The table below summarizes major CBT techniques and their practical benefits.
CBT techniques and their practical benefits: This comparison shows how CBT’s modular techniques address different anxiety mechanisms.
The next section outlines specific CBT practices for generalized anxiety that you can practice or discuss with a clinician.
What Are the Key CBT Techniques for Managing Generalized Anxiety?
CBT for generalized anxiety focuses on interrupting chronic worry cycles, testing anxious predictions, and reconnecting with valued activities to break avoidance. Cognitive restructuring teaches you to map automatic thoughts, weigh evidence for and against anxious predictions, and create balanced alternatives—one simple practice is keeping a brief thought record after a worry episode. Behavioral experiments and worry exposure test feared outcomes directly—plan a small, observable test and review what happened—to weaken the link between worry and threat. Behavioral activation counteracts withdrawal by scheduling purposeful activities and tracking mood to reinforce pleasure and mastery, while relaxation or grounding skills offer short‑term relief during spikes of anxiety. These techniques change both thinking and behavior; next we describe ways to adapt CBT so it’s culturally attuned for LGBTQ+ and BIPOC clients.
How Is Affirmative CBT Tailored for LGBTQ+ and BIPOC Individuals?
Affirmative CBT modifies standard cognitive and behavioral techniques to reflect minority stress, identity‑related beliefs, and culturally specific stressors. Clinicians weave minority stress frameworks into case formulations, explicitly address identity‑linked thoughts—like internalized stigma or anticipatory vigilance—and design behavioral experiments with identity safety and community context in mind. Affirming language, attention to culturally grounded values, and therapist humility about social determinants of health foster trust and engagement for LGBTQ+ and BIPOC clients. Skilled therapists adapt homework and exposure tasks to relevant settings and risks to avoid retraumatization and make goals personally meaningful. These culturally aware adaptations also create natural bridges to other methods—like ACT—that emphasize values and acceptance when worry is persistent.
Adapting Affirmative Cognitive Behavioral Therapy for LGBTQ+ Youth via Telehealth
Telehealth expands opportunities for social workers and clinicians to deliver effective, affirmative CBT to marginalized youth, including LGBTQ+ populations. The pandemic accelerated telehealth adoption, and while ethical and legal guidance exists, there is less specific direction on translating in‑person clinical skills to virtual care for LGBTQ+ youth. This paper shares practical examples from implementing AFFIRM—a group‑based affirmative CBT intervention—via telehealth: it outlines key considerations for online delivery, details clinical skills and strategies that support success, walks through a case adaptation of cognitive restructuring with a transgender youth, and offers concrete guidance clinicians can use when moving affirmative CBT to a virtual setting.
How Does Acceptance and Commitment Therapy Support Anxiety Relief?
Acceptance and Commitment Therapy (ACT) helps reduce the impact of anxiety by changing how people relate to anxious thoughts and sensations instead of trying to eliminate them. ACT uses acceptance, cognitive defusion, values clarification, and committed action: you learn to notice thoughts without getting fused to them, make space for uncomfortable internal experiences, and choose behaviors that align with what matters most. These shifts lower experiential avoidance and restore functioning. Research and clinical practice show ACT works well for chronic worry and stress—especially when avoidance keeps distress going—and it can be combined with exposure or skills training for broader effect. Below we explain how mindfulness and values work in ACT and how those processes help with persistent worry.
ACT focuses on practical processes you can practice in a therapy session and apply daily—mindful awareness and concrete, values‑driven goals—which the next section presents as short exercises.
What Role Do Mindfulness and Values Play in ACT for Anxiety?
Mindfulness in ACT builds present‑moment awareness and a nonjudgmental stance toward anxious thoughts, so thoughts can be noticed without automatic avoidance. Values clarification helps you identify what matters—relationships, creativity, community—and then commit to small, achievable actions that reflect those values even when anxiety is present. Short practices include a simple “observe the breath” exercise to notice the thought–feeling cycle and a values‑sorting activity that lists life domains and ranks what’s most important to guide committed actions. Regular practice creates momentum for exposure and behavioral change; the next subsection shows how ACT uses defusion and committed action to address persistent worry.
How Can ACT Help Manage Chronic Worry and Stress?
ACT reduces chronic worry through defusion techniques—labeling thoughts as “just thoughts” or repeating a worry phrase until it loses charge—so repetitive cognitions have less control. Acceptance exercises teach making room for unpleasant sensations while still engaging in valued actions, breaking the avoidance–anxiety cycle. Committed action planning turns big values into specific, measurable steps, increasing activity and creating evidence that anxiety doesn’t always dictate outcomes. Combining defusion, acceptance, and action builds resilience: many people report better functioning before full symptom remission, reflecting ACT’s emphasis on living a meaningful life alongside ongoing symptoms. From ACT, exposure offers direct ways to reduce fear responses and avoidance.
What Is Exposure Therapy and When Is It Effective for Anxiety?
Exposure therapy is a behavioral method that reduces fear and avoidance by systematically confronting feared stimuli in a safe therapeutic context to promote habituation and new learning. It’s especially effective for specific phobias, panic disorder with agoraphobia, social anxiety, and post‑traumatic stress when tailored appropriately; the mechanism emphasizes inhibitory learning—forming new, safer associations rather than erasing fear memories. Exposure can be in vivo (real life), imaginal (structured visualization), interoceptive (eliciting bodily sensations), or delivered via Virtual Reality (VR), and clinicians choose the format based on the target anxiety and practical constraints. Good exposure work includes building a hierarchy, setting measurable exposures, repeating practice, and mental health professional guidance to manage safety and comorbidities. The next sections explain hierarchy building and VR’s role in exposure.
Below are common exposure formats and typical clinical uses.
In Vivo Exposure: Real‑life practice confronting feared situations with therapist guidance.
Imaginal Exposure: Structured recall or visualization for trauma or situations that can’t be recreated.
Interoceptive Exposure: Safely inducing bodily sensations to reduce fear of those sensations (useful in panic).
Virtual Reality Exposure: Controlled simulated environments that approximate feared stimuli.
These formats show exposure’s flexibility; the following subsection describes how to construct a gradual hierarchy for phobias.
How Do Gradual Exposure Techniques Work for Phobias?
Gradual exposure starts with a collaboratively built fear hierarchy that ranks situations from least to most distressing. Treatment moves through repeated, controlled exposures beginning with lower‑intensity items to build confidence and new learning. Therapists help design exposures with clear, observable success criteria—like tolerating a stimulus for a set time—and encourage repetition until distress meaningfully decreases. Safety behaviors that interfere with learning are removed gradually so clients can experience that feared outcomes are unlikely or manageable. Progress is tracked using subjective units of distress and functional gains. For example, a public‑speaking hierarchy might begin with reading a paragraph to a trusted friend and progress to presenting to a small group—measurable steps toward mastery. Next, we consider technological tools like VR that can complement in‑person practice.
What Are the Benefits and Considerations of Virtual Reality Exposure Therapy?
Virtual Reality (VR) exposure creates a controllable, repeatable simulation of feared situations and can improve access when real‑world exposures are impractical or unsafe. Research indicates VR can yield results comparable to in‑person exposure for some phobias and social anxiety. VR allows precise stimulus control, scalable intensity, and repeated practice in clinic sessions; however, it requires trained clinicians, equipment, and ethical oversight so simulations don’t overwhelm clients. Considerations include cost, suitability for the specific fear, and how VR integrates with real‑world practice—VR usually supplements rather than replaces in vivo work. Clinicians also monitor for cybersickness and obtain informed consent. Knowing these advantages and limits helps you choose the right exposure modality and prepares you to explore other therapy options that address anxiety through different mechanisms.
What Other Therapy Types Are Effective for Anxiety Relief?
Beyond CBT, ACT, and exposure, several therapies address anxiety through emotion regulation, relationships, or deeper pattern work—valuable options when anxiety relates to attachment, trauma, or complex emotion dysregulation. Dialectical Behavior Therapy (DBT) teaches skills in mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness, useful when anxiety co‑occurs with intense reactivity. Psychodynamic therapy explores relational patterns and unconscious drivers of chronic anxiety to build insight, while Interpersonal Therapy (IPT) focuses on role transitions and relationship conflicts that trigger or sustain anxiety. Mindfulness‑Based Cognitive Therapy (MBCT) blends mindfulness with relapse‑prevention strategies for rumination and co‑occurring depression, and trauma‑informed approaches adapt pacing and safety for those with trauma histories. The table below compares key therapies, common use cases, and primary techniques to help you match your needs to therapeutic styles.
Comparative overview of additional therapy types:
DBT is used for: Anxiety with strong emotional reactivity, self‑harm risk, or impulsivity. Key techniques: Structured skills training — mindfulness, distress tolerance, emotion regulation.
Psychodynamic Therapy is used for: Longstanding anxiety tied to relational patterns or early attachment issues. Key techniques: Exploration of unconscious conflicts, transference, and insight‑oriented work.
Interpersonal Therapy (IPT) is used for: Anxiety linked to role changes, grief, or relationship conflict. Key techniques: Time‑limited focus on interpersonal problem areas and practical skill building.
MBCT is used for: Recurrent anxiety with depressive features or persistent rumination. Key techniques: Structured mindfulness practices combined with cognitive strategies.
How Does Dialectical Behavior Therapy Help with Emotional Regulation in Anxiety?
DBT helps manage anxiety by teaching concrete skills that reduce emotional reactivity and increase tolerance for intense sensations that often amplify worry. Mindfulness skills build moment‑to‑moment awareness without judgment so early signs of escalation are noticed sooner; distress tolerance techniques offer immediate ways to get through intense episodes without relying on avoidance. Emotion regulation modules help identify and change vulnerable patterns—like heightened sensitivity to criticism—that fuel anxiety, while interpersonal effectiveness work reduces relationship stressors that trigger worry. Practicing these skills in structured modules and applying them to real‑life situations helps clients stabilize affect and engage more fully in exposure or values‑based action, connecting skills training with deeper therapeutic goals.
What Are Psychodynamic and Interpersonal Therapy Approaches for Anxiety?
Psychodynamic therapy views anxiety as often rooted in unresolved conflicts, attachment ruptures, or internalized relational expectations, and uses exploration of past relationships and patterns to generate insight and change. Through reflective dialogue and attention to transference, clients identify repetitive themes—such as fear of abandonment or perfectionism—that shape anxious responses and interpersonal behavior. Interpersonal Therapy (IPT) is a time‑limited, problem‑focused approach that reduces anxiety by addressing current relationship stressors, role transitions, or bereavement, and by building communication and problem‑solving skills. Both approaches may take longer than skills‑focused therapies but can produce deep, lasting changes in how anxiety is generated and maintained, complementing skills work and exposure by tackling interpersonal and developmental roots of distress.
How Do You Find the Right Affirming Therapist for Anxiety in NY and NJ?
Finding an affirming therapist means checking clinical approach, cultural competence, logistics, and cost—especially for LGBTQ+ and BIPOC adults seeking identity‑affirming care in New York and New Jersey. Start with a practical checklist for searches and first contacts: confirm experience with anxiety‑specific treatments, ask about affirmative work with LGBTQ+ and BIPOC clients, verify remote availability for cross‑jurisdiction options, and learn about intake and matching processes to ensure a good fit. Look for clinicians who describe minority stress competency, collaborative goal setting, and transparent information about fees and insurance; an intake conversation should cover both symptom targets and identity‑related safety. Considering in‑network participation and sliding scale options lowers financial barriers, and remote weekly psychotherapy expands access across regions. The next subsection offers concrete guidance on insurance and affordability.
Checklist for selecting an affirming therapist:
Clinical Fit: Confirm training and experience with anxiety‑focused approaches such as CBT, ACT, psychodynamic, or exposure therapy.
Affirming Competence: Verify explicit experience or specialization in LGBTQ+ and BIPOC‑affirming care.
Logistics: Ensure availability for remote weekly psychotherapy and clarify session frequency and format.
Affordability: Ask about in‑network insurance participation, sliding scale options, and intake/matching services.
This checklist helps you prioritize both practical and cultural fit. The following section details insurance options and affordability considerations for clients in NY and NJ.
What Should You Know About Navigating Insurance and Affordable Therapy Options?
Knowing insurance and payment options reduces barriers to starting therapy and helps you plan financially for ongoing care in New York and New Jersey. Many clinicians accept major insurers; common in‑network options to confirm include Aetna, Anthem, Optum, Humana, MetroPlus Health, and Wellfleet, though network participation varies by clinician and plan—always verify benefits before scheduling. Sliding scale fees are often available for qualifying clients, and remote services can expand the pool of therapists who accept your plan or offer lower rates across state lines. The table below summarizes insurer and payment options with practical verification steps so you can approach intake calls with clear questions.
Insurance and payment options overview:
Aetna: Network varies by clinician. Confirm mental health coverage and any prior authorization rules.
Anthem: Varies by clinician. Check provider directories and session limits for outpatient therapy.
Optum: Varies by clinician. Verify network participation and telehealth coverage across NY/NJ.
Humana: Varies by clinician. Ask about behavioral health carve‑outs and out‑of‑network reimbursement.
MetroPlus Health: Varies by clinician. Review plan‑specific behavioral health benefits and provider lists.
Wellfleet: Varies by clinician. Confirm outpatient therapy approvals and any required referrals.
Sliding scale: Network N/A. Ask clinicians about income‑based reduced fees and eligibility criteria.
After checking coverage, contact the provider’s intake team to confirm real‑time eligibility. The next subsection explains how remote therapy can broaden access and what to expect from a matching or intake process. (Note: NYC Affirmative Psychotherapy offers in-network therapy for all of the above insurance networks.)
What Are the Benefits of Remote Online Therapy for Anxiety Relief?
Remote therapy increases access to mental health professionals with specific affirming skills regardless of location, allowing adults in NY and NJ to connect with therapists experienced in LGBTQ+ and BIPOC‑affirming care when local options are limited. Evidence supports teletherapy’s effectiveness for anxiety, and remote weekly sessions promote continuity by removing travel barriers, offering scheduling flexibility, and enabling practice in real‑life settings. Practical tips: create a private, distraction‑free space; use headphones for confidentiality; test your tech ahead of time; and agree on a safety plan with your clinician for crisis situations. Remote services also make client‑matching easier, pairing you with therapists who understand your identity and clinical needs—smoothing the path to effective anxiety‑focused work.
These remote advantages lead naturally to how affirmative therapy principles specifically support anxiety relief for marginalized communities.
How Does Affirmative Therapy Support Anxiety Relief for LGBTQ+ and BIPOC Communities?
Affirmative therapy centers identity‑affirming practices that validate lived experience, address minority stressors, and adapt interventions to cultural contexts—strengthening alliance and improving outcomes for LGBTQ+ and BIPOC clients. Culturally sensitive care acknowledges structural contributors to anxiety—like discrimination, microaggressions, and social marginalization—and weaves those realities into case formulation and treatment planning rather than pathologizing adaptive responses. Affirming clinicians use identity‑affirming language, tap community‑based coping resources, and co‑design exposures and behavioral experiments that prioritize cultural safety. For people seeking services, QPOC‑founded therapist communities and streamlined client‑matching can increase trust and relevance; the following paragraphs explain why these elements matter and where to find supportive resources.
LGBTQ+ Affirmative Therapy: Navigating Sociopolitical Contexts for Culturally Responsive Care
Providing affirming, culturally responsive care to LGBTQ+ clients requires clinicians to attend to a shifting sociopolitical landscape. Laws, policies, and public discourse can have immediate effects on the health and safety of LGBTQ+ people—both directly and indirectly—through increased polarization, strained family relationships, and higher rates of discrimination and victimization, all of which can worsen mental health. This volume aims to deepen understanding of stressors that disproportionately affect LGBTQ+ communities, highlight their strengths, and offer practical implications for case conceptualization and treatment. We hope readers finish each chapter better prepared and more confident in delivering LGBTQ+ affirmative care, and that the book serves as a useful resource for clinicians and training programs.
What Makes Culturally Sensitive Anxiety Therapy Important for BIPOC Individuals?
Culturally sensitive therapy improves engagement, trust, and retention by recognizing systemic stressors, cultural values, and community strengths that shape anxiety and recovery. When therapists use culturally adapted interventions—such as contextualized case formulations, family‑ or community‑centered strategies, and respect for culturally specific expressions of distress—clients commonly report stronger rapport and more practical progress. Research and clinical guidance show that acknowledging discrimination and validating culturally based coping reduces shame and increases willingness to try exposure or skills practice. Tailoring interventions to cultural realities helps BIPOC clients translate therapeutic gains into safer engagement at work, school, and in family relationships, and it supports community‑specific referral pathways and resources discussed next.
Where Can LGBTQ+ Individuals Find Affirming Mental Health Resources for Anxiety?
LGBTQ+ people can find affirming mental health resources through specialized directories, community organizations, and therapist‑matching services that screen for sexual orientation and gender identity competency, as well as by reviewing clinician statements about affirmative practice. Good questions to ask include a therapist’s approach to minority stress, examples of past work with LGBTQ+ clients, and whether they connect clients to identity‑affirming referrals or groups. Community‑based resources also offer peer supports that complement individual therapy. For streamlined access, client‑matching services that include QPOC‑founded networks and clinicians experienced with LGBTQ+ and BIPOC clients can reduce search friction and improve safety. This pathway makes it easier to start remote weekly psychotherapy or schedule an initial consultation with a provider whose values and expertise fit your needs.
Integration note: NYC Affirmative Psychotherapy LCSW PLLC is a QPOC‑founded community of clinicians providing remote weekly psychotherapy for adults in NY and NJ, using a client‑matching approach to connect people with therapists who understand their needs. The practice emphasizes culturally sensitive, affirming care for LGBTQ+ and BIPOC clients, offers affordability options including in‑network participation with major insurers and sliding scale fees, and uses a streamlined online intake and matching process to schedule initial consultations. If you’re ready to take next steps, confirm your insurance benefits and complete an intake to be matched with a clinician who specializes in anxiety treatment.